Food allergies and intolerances are increasingly common in today’s society, affecting millions of people worldwide. While often used interchangeably, food allergies and intolerances are distinct conditions that require different approaches for management. Understanding the differences between the two, as well as recognizing the symptoms, is crucial for maintaining overall health and well-being. This article delves into the complexities of food allergies and intolerances, exploring the underlying immune responses, contributing genetic and environmental factors, and the impact these conditions can have on both physical and mental health. Additionally, we’ll discuss practical strategies for managing these challenges in daily life, including tips for navigating social situations and staying informed on the latest research and treatment options.
Delve into this topic with zopmj.com to gain a thorough understanding.
1. Common Food Allergies and Their Symptoms
Food allergies arise when the immune system misinterprets a harmless food protein as a danger, triggering a variety of symptoms that can range in severity. The most frequent food allergens include peanuts, tree nuts, shellfish, fish, milk, eggs, soy, and wheat. These foods account for the majority of allergic reactions, which can present as hives, itching, swelling of the lips, face, or throat, abdominal pain, nausea, vomiting, diarrhea, and in extreme cases, anaphylaxis—a potentially fatal reaction demanding immediate medical intervention.
Food allergies are more common in children, and while some allergies, such as those to milk or eggs, often disappear as they grow older, others, like peanut or shellfish allergies, can last a lifetime. Recognizing the unique symptoms of each food allergy is crucial for prompt treatment and management.
For example, individuals with a peanut allergy may experience symptoms ranging from mild skin reactions to severe anaphylaxis within minutes of exposure. In contrast, a milk allergy might lead to gastrointestinal discomfort or skin issues in children. It’s important to remember that symptoms can vary not only between individuals but also for the same individual over time. Recognizing the early signs of a food allergy and understanding which foods are most commonly involved can help manage these reactions and prevent serious consequences.
2. Differences Between Food Allergies and Intolerances
Food allergies and food intolerances are often confused, but they are distinct conditions with different bodily responses and health implications. A food allergy is an immune system reaction that occurs when the body misidentifies a food protein as a threat. This triggers an immune response, resulting in symptoms ranging from mild, such as hives or itching, to severe, such as anaphylaxis. Even minute amounts of the allergenic food can cause a reaction, and the effects are usually immediate or appear within a few hours of consumption.
Food intolerance, however, does not involve the immune system. Instead, it is typically a digestive issue where the body struggles to break down certain foods, such as lactose or gluten. Symptoms of food intolerance tend to be milder than those of food allergies and may include bloating, gas, stomach cramps, or diarrhea. These symptoms often develop gradually and are dose-dependent, meaning increased consumption of the problematic food is necessary to cause discomfort.
Recognizing the distinctions between food allergies and food intolerances is essential for accurate diagnosis and treatment. Food allergies demand complete avoidance of the trigger, whereas food intolerances may permit limited consumption of the offending food or the use of digestive support products.
3. Understanding the Immune Response in Food Allergies
Food allergies involve an intricate immune response where the body’s defenses mistakenly identify specific proteins in certain foods as harmful. When someone with a food allergy eats an allergenic food, their immune system recognizes the protein as an invader. This triggers the production of immunoglobulin E (IgE) antibodies, which attach to the food proteins. Subsequent exposures to the allergen cause these antibodies to activate immune cells, leading to the release of histamine and other chemicals, ultimately resulting in an allergic reaction.
These reactions can manifest in a variety of ways, from mild symptoms like itching or hives to severe responses such as anaphylaxis, which can be life-threatening. The severity of the reaction is often determined by the individual’s sensitivity and the amount of the allergen consumed. Understanding this immune mechanism is essential for recognizing and managing food allergies, as it underscores the body’s ability to mount a rapid and intense immune response.
4. Genetic and Environmental Factors Contributing to Food Allergies
Both genetic and environmental factors play significant roles in the development of food allergies. Genetics contribute to a person’s likelihood of developing food allergies, particularly if there is a family history of allergies, asthma, or eczema. Individuals with parents or siblings who have these conditions are at a higher risk of experiencing similar allergic reactions.
Environmental factors also influence the onset and prevalence of food allergies. Early exposure to potential allergens, such as through diet or the environment, can either increase or decrease the risk, depending on timing and quantity. For instance, introducing allergenic foods like peanuts to infants at an appropriate age may reduce the risk of developing allergies later in life. Additionally, environmental changes, such as increased pollution and altered microbiomes due to modern hygiene practices, have been linked to a rise in allergic conditions.
The interplay between genetics and environment underscores the complexity of food allergies, requiring both preventative measures and personalized management strategies to mitigate risks.
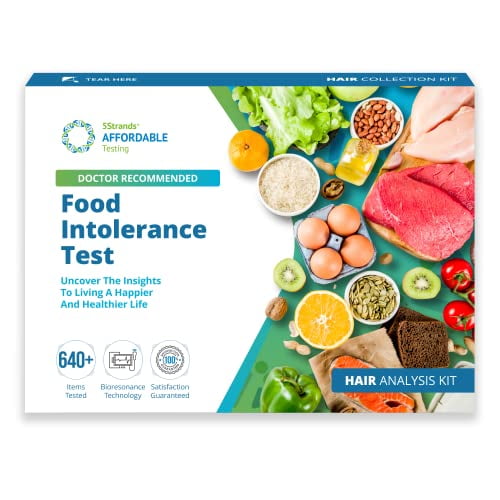
5. Diagnosis and Testing for Food Allergies and Intolerances
Pinpointing the cause of food allergies and intolerances necessitates a multifaceted approach, incorporating medical history, symptom tracking, and specialized tests. When it comes to food allergies, the journey often commences with a comprehensive dialogue between the patient and a healthcare provider, delving into symptoms, dietary patterns, and family history. Skin prick tests, a common diagnostic tool, involve introducing minute quantities of potential allergens to the skin and observing for any reactions. Blood tests, specifically those measuring IgE antibody levels, can further solidify the presence of a food allergy.
When food intolerances are suspected, elimination diets are often recommended. This involves removing suspected foods from the diet for a specific time and then gradually reintroducing them while carefully monitoring for any symptoms. For example, lactose intolerance can be diagnosed through a hydrogen breath test, which measures the body’s ability to properly digest lactose.
Effective management relies on accurate diagnosis, which is crucial for distinguishing between food allergies and food intolerances. Food allergies necessitate strict avoidance and emergency preparedness, while food intolerances may allow for more adaptable dietary modifications.
6. Managing Food Allergies in Daily Life
Managing food allergies in daily life requires careful planning and vigilance to avoid exposure to allergens while maintaining a balanced diet. The first step is to read food labels meticulously, as even trace amounts of an allergen can trigger a reaction. Many countries have labeling laws that require the disclosure of common allergens, but it’s essential to stay updated on potential cross-contamination risks, especially with processed foods.
At home, preventing cross-contact is key. This includes using separate utensils, cookware, and preparation areas for allergen-containing foods. For those with severe allergies, carrying an epinephrine auto-injector at all times is crucial in case of accidental exposure.
Eating out presents additional challenges, but informing restaurant staff about food allergies and asking detailed questions about meal preparation can help reduce risks. It’s also beneficial to have a support network, including family, friends, and co-workers, who understand the seriousness of food allergies and can assist in maintaining a safe environment. With these precautions, individuals can effectively manage their food allergies while leading a fulfilling life.
7. Nutritional Challenges and Solutions for Those with Food Allergies
Food allergies pose significant nutritional challenges, as individuals may be required to avoid common foods, potentially limiting their intake of essential nutrients. For example, individuals with a milk allergy who avoid dairy products may experience deficiencies in calcium and vitamin D. Likewise, eliminating nuts or soy from the diet can impact the intake of protein, healthy fats, and other essential nutrients.
To tackle these challenges, it is crucial to explore alternative sources of essential nutrients. For calcium, individuals with dairy allergies can opt for fortified plant-based milk alternatives, such as almond, oat, or rice milk, and incorporate leafy green vegetables, fortified cereals, and tofu into their diet. For protein, those avoiding nuts and soy can include alternatives such as lean meats, poultry, fish, legumes, and seeds in their meals.
A registered dietitian can help create a balanced meal plan that addresses nutritional deficiencies. They offer guidance on appropriate substitutions and supplements to ensure your nutritional needs are met. Furthermore, exploring fortified foods and carefully reading food labels can also contribute to a well-rounded diet.
For optimal health and well-being, maintaining nutritional balance is critical. This makes proactive dietary planning and professional guidance essential for individuals managing food allergies.
8. Impact of Food Allergies on Mental and Emotional Health
Food allergies can significantly impact mental and emotional health, often causing stress, anxiety, and social isolation. The constant need to avoid allergens and the fear of accidental exposure can lead to heightened anxiety and worry. This anxiety is not only related to the immediate risk of an allergic reaction but also the potential long-term health implications.
The social aspects of food allergies can also be challenging. Individuals with severe allergies may find it difficult to participate in social events or eat out, leading to feelings of exclusion or frustration. This can impact self-esteem and contribute to a sense of isolation from peers and family.
Children with food allergies may experience additional psychological stress, including bullying or teasing, which can affect their emotional well-being and social development. Parents and caregivers also face emotional strain as they manage their child’s condition and navigate various social situations.
Support groups and counseling can be valuable resources for managing these emotional challenges. Connecting with others who have similar experiences can provide comfort and practical advice. Additionally, professional mental health support can help individuals and families develop coping strategies and address any emotional or psychological impacts of living with food allergies.
9. Latest Research and Advances in Food Allergy Treatments
Recent advancements in food allergy research are paving the way for more effective treatments and management strategies. One of the most promising developments is oral immunotherapy (OIT), which involves gradually introducing small, controlled amounts of the allergen into the patient’s diet to build tolerance over time. This approach aims to desensitize the immune system and reduce the severity of allergic reactions. Clinical trials have shown that OIT can significantly improve the quality of life for individuals with food allergies, though it requires careful medical supervision.
Another notable advancement is the development of biologic medications, such as monoclonal antibodies, which target specific immune responses involved in food allergies. These treatments are designed to interrupt the allergic reaction process and provide relief from severe symptoms. Dupixent, for example, has been approved for treating eosinophilic esophagitis, a condition linked to food allergies.
In addition, researchers are exploring potential vaccines that could provide long-term protection against food allergies. These vaccines aim to retrain the immune system to tolerate allergens without triggering adverse reactions.
Ongoing studies and clinical trials continue to refine these treatments and investigate new options, offering hope for more effective and sustainable solutions for managing food allergies in the future.
10. Practical Tips for Eating Out with Food Allergies and Intolerances
Dining out with food allergies or intolerances demands meticulous planning and communication to guarantee safety. Begin by researching restaurants ahead of time to identify those with experience accommodating food allergies or providing allergen-free options. Many restaurants provide allergen information online, which can aid in choosing suitable establishments.
When dining out, always be sure to inform the restaurant staff about any allergies or intolerances you may have. Clearly communicate the specific foods you need to avoid, and ask detailed questions about the preparation of meals to prevent cross-contamination. If necessary, request to speak with the chef or manager for further clarification.
Carrying a food allergy card is a good idea. It lists your allergies and symptoms, which can be helpful in an emergency. It’s also a good practice to bring safe snacks with you. This ensures you have alternatives if your food choices are limited.
Ultimately, trust your gut feeling. If you have any reservations about the safety of the food or the restaurant’s ability to meet your requirements, it’s wisest to play it safe and select a different eatery.
Understanding and managing food allergies and intolerances is crucial for maintaining health and well-being. By recognizing symptoms, differentiating between allergies and intolerances, and implementing effective management strategies, individuals can reduce risks and enhance their quality of life. Ongoing research and practical tips further support safe and informed choices.
zopmj.com